Kampala ‒ In Uganda, more than 1.4 million people are living with HIV and of these, 5.8% have diabetes. Diabetes is common among people living with HIV and is one of the main causes of death in this population. Overall, non-communicable diseases account for 36% of annual deaths in the country.
Diabetes occurs when the body does not produce enough insulin or is unable to use insulin, the hormone that regulates blood glucose.
To address this health threat, Uganda is implementing a programme to integrate care for noncommunicable diseases into HIV services. Launched in 2019, the programme aims to improve the prevention, timely diagnosis and long-term management of chronic diseases among people living with HIV.
A strong collaboration between the Ugandan government, World Health Organization (WHO), United Nations Development Programme and the United States President's Emergency Plan for AIDS Relief has enabled the mobilization of over US$ 6 million to scale up the implementation of the programme in 2022 and 2023. These efforts, along with better access to HIV treatment, have led to a decline in the number of deaths among people living with HIV, from 24 245 deaths in 2017 to 16 450 in 2023.
Fourteen years later, in 2012, Byaruhanga discovered that he had diabetes when he was receiving treatment at the institute after he suffered a stroke. Diabetes is a risk factor for stroke.
“When I had a stroke 11 years ago, the nurse discovered that my sugar level was high. I was immediately put on treatment and was recommended to meet a diabetes specialist at another hospital,” he says. “However, it was challenging going between two physicians from different health facilities at the same time.”
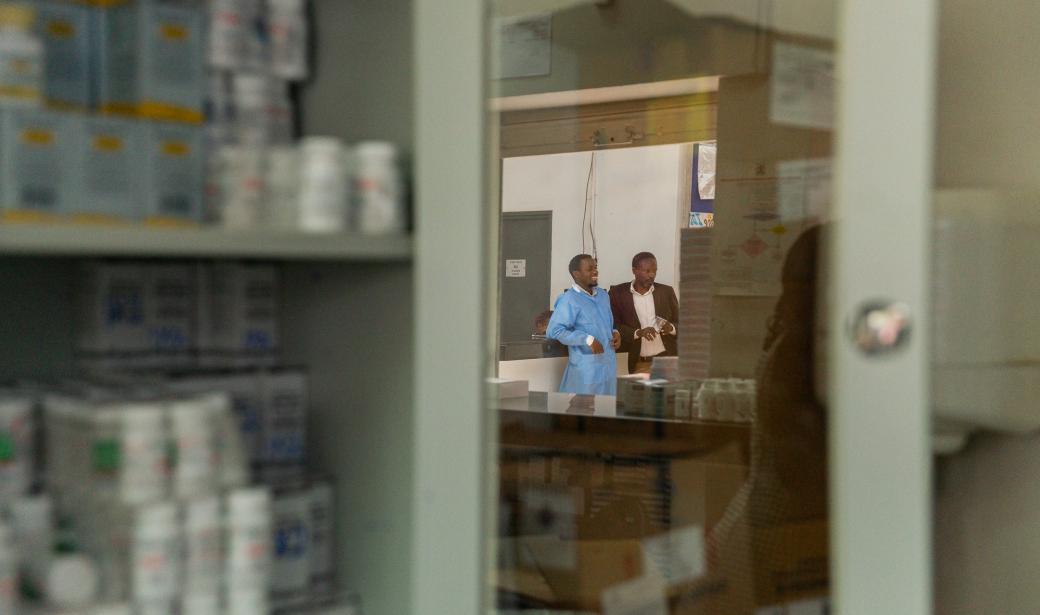
“Through our noncommunicable disease/HIV initiative, we are seeing a reduction in diabetes-related complications among clients, as the disease is detected early, facilitating timely client management,” explains Dr Noella Owarwo, a physician and Deputy Director of Infectious Diseases Institute (IDI).
"The exchanges I have with the doctor when he escorts me [to the consultation room] make me feel better. I feel accepted and respected," she says.
One of the features of the noncommunicable disease /HIV initiative is the ability to manage noncommunicable diseases that are more common among people living with HIV. Over 1800 HIV centres across the country are equipped with service providers with the capacity to screen and manage cervical cancer, diabetes and hypertension.
"The management of noncommunicable diseases among HIV-positive people, using WHO guidelines and tools, has led to remarkable results,” says Dr Franck Mugabe, Principal Medical Officer ‒ Noncommunicable Diseases at the Ministry of Health. “The country has decreased deaths among people living with HIV by almost one-third since 2017 to date.”
Uncontrolled blood sugar for a long period damages the nerves and impairs their function, leading to health problems ranging from mild numbness to pain that makes it hard to do normal activities.
“During my consultations, Dr Owarwo explains how to control my nerve function and prescribes a diet that I'm following to remain healthy," explained Byaruhanga.
“Since 2019 I've been receiving HIV and diabetes medication together, without interruption, and I've never been admitted to hospital,” he says.
Good health means that Byaruhanga can continue following his passion as a peer educator at a nearby health centre, where he encourages his peers to adhere to their HIV treatment. He also founded a theatre group called “Karibobo" at the institute through which his peers support each other through dance, poems and drama.
“The lessons learned in the implementation of this intervention should be scaled up to include everyone and continued investments is critical. WHO is ready to support this process,” says Dr Hafisa Kasule, WHO technical officer in charge of noncommunicable diseases.
Communications Officer
WHO Uganda
Email: tcheutchouae [at] who.int (tcheutchouae[at]who[dot]int)
Media Relations Officer
WHO Regional Office for Africa
Email: dalalm [at] who.int (dalalm[at]who[dot]int)
Tel: +254 703 245 761 (WhatsApp)