Bridging immunity gaps: Nigeria’s fight against Poliovirus in high-risk communities
Maiduguri, 13 March, 2025 - In Jere Local Government Area (LGA) of Borno State, four-year-old Amina* from Mairi Ward in Buladina settlement has received intermittent immunization since birth. Despite multiple vaccination efforts, she has missed several recommended doses for her age, leaving her vulnerable to poliovirus infection.
“Amina missed some doses because we are often not around when they conduct the vaccination campaigns,” said her mother, Saratu Bulama* (*names changed for privacy).
Amina’s story reflects Nigeria’s ongoing challenges in halting poliovirus transmission and other vaccine-preventable diseases, particularly in hard-to-reach and conflict-affected areas.
Tackling Circulating Variant Poliovirus Type 2 (cVPV2)
Halting the transmission of circulating variant poliovirus type 2 (cVPV2) remains a national priority for Nigeria. Despite significant efforts to vaccinate every child under five, cVPV2 transmission persists. Between January 2024 and 10 March 2025, Nigeria reported 122 confirmed cVPV2 cases across 15 states, including 10 cases in 2025 alone.
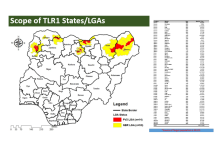
The National Primary Healthcare Development Agency (NPHCDA), under the coordination of the National Emergency Operations Centre (NEOC) and in collaboration with the World Health Organization (WHO), has adopted the Targeted Local Outbreak Response (TLR) strategy to address immunity gaps and curb the virus’s spread. The strategy focuses on high-risk areas aiming to vaccinate all susceptible children and interrupt transmission.
A recent four-day vaccination campaign targeted 3.8 million children across seven high-burden states: Borno, Jigawa, Kano, Kebbi, Sokoto, Yobe, and Zamfara. By the campaign’s end, over 3.6 million children had received the novel oral polio vaccine type 2 (nOPV2). However, challenges remain—some children were missed due to caregiver noncompliance or absence during vaccination rounds.
Dr Abdulkadir Usman Gana, NEOC Incident Manager, acknowledged the gaps: “While it’s encouraging to see the high number of children reached, we must intensify social mobilization and refine our strategies to address vaccine hesitancy and missed children. Our goal is to ensure no child is left behind in our efforts to interrupt cVPV2 transmission
Targeted Interventions for Maximum Impact
The NEOC operations working group, coordinated by WHO, plays a critical role in planning and monitoring TLR campaigns. The group employs a data-driven approach, triangulating surveillance data, routine immunization records, and polio laboratory results to define the scope of each response. Planning parameters include analysing pending cVPV2 isolates in LGAs, the timing of the most recent cases, population immunity levels (via household surveys), risk status of neighbouring LGAs and wards, target population estimates, vaccine availability, and logistical needs.
Dr Walter Kazadi Mulombo, WHO Country Representative in Nigeria, praised the TLR approach as a rapid-response mechanism to contain poliovirus spread. “The targeted nature of TLR allows for better supervision and high-quality execution,” he said. “We have a critical opportunity to turn the tide against cVPV2, and now is the time to act decisively. WHO remains committed to supporting Nigeria, despite funding constraints.”
Mobilizing Communities for Success
WHO supported the implementing states throughout the campaign, from planning to execution. This included training over 18,727 health workers, facilitating coordination meetings before and after daily vaccination activities, and developing tracking systems to ensure adherence to immunization schedules in targeted areas. WHO deployed over 6,000 personnel across national, state, LGA, and ward levels to support planning and implementation.
“We supported the coordination and supervision of vaccination teams, including logistics payments,” said Dr Yusuf Muhammad Argungu, WHO State Coordinator for Sokoto State. “WHO also facilitated advocacy and communication activities through our extensive network of personnel across LGAs and wards.”
Community engagement was key. Zayyanu Adamu, a field volunteer in Maiyama LGA, Kebbi State, explained: “I worked with the ward focal person to organise community dialogues, sensitising residents about the vaccine’s importance. During the campaign, I collaborated with the village head to resolve cases of noncompliance and child absence, which boosted our success rate in the ward.”
Measuring Impact Through Quality Assurance
To validate vaccination coverage data, WHO supported the states in conducting Lot Quality Assurance Surveys (LQAS). Independent professionals, including medical doctors and university lecturers, were deployed to randomly selected wards and settlements. Surveyors visited 10 random households per area, verifying the vaccination status of a randomly selected child within the target age group.
The LQAS results were promising: 97% of surveyed LGAs achieved over 90% vaccination coverage, indicating strong campaign performance in most areas.
Looking Ahead: Sustained Efforts to End cVPV2
Nigeria is planning another TLR phase starting 12 March 2025, targeting 946,600 children across five states: Jigawa, Oyo, Sokoto, Yobe, and Zamfara. These efforts aim to further close immunity gaps and sustain progress against cVPV2.
While challenges like vaccine hesitancy and logistical barriers persist, the collaboration between NPHCDA, NEOC, WHO, and local communities demonstrates Nigeria’s commitment to protecting every child from poliovirus. With continued innovation, community trust, and global support, Nigeria is on a path toward a polio-free future.